- Our Team
- For Patients
- Treatments & Services
- Medical Professionals
Laryngeal
Laryngeal
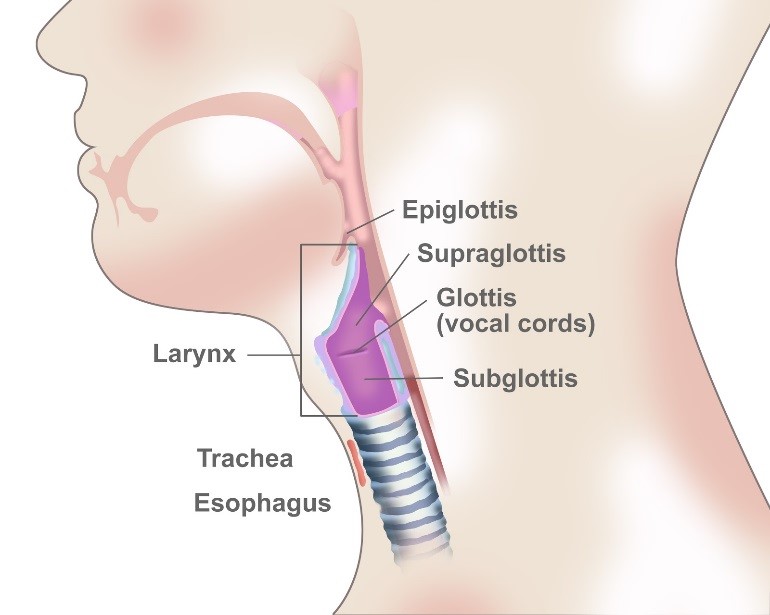
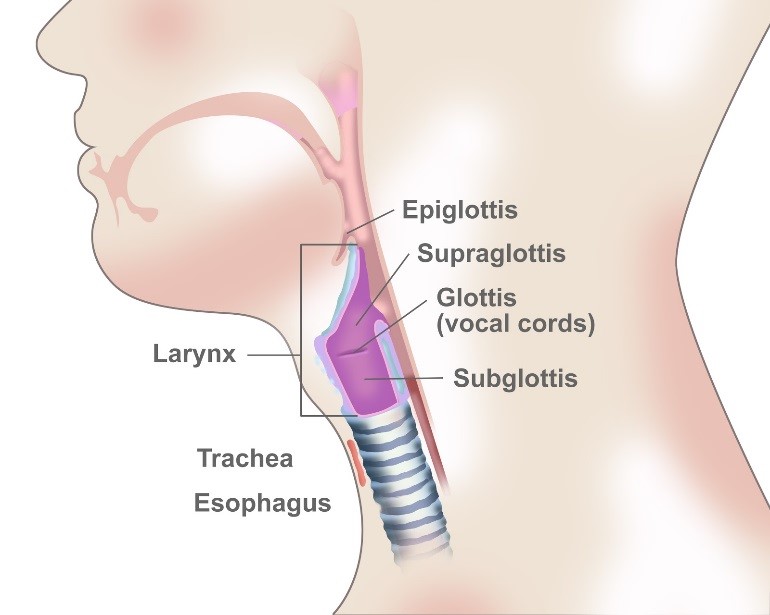
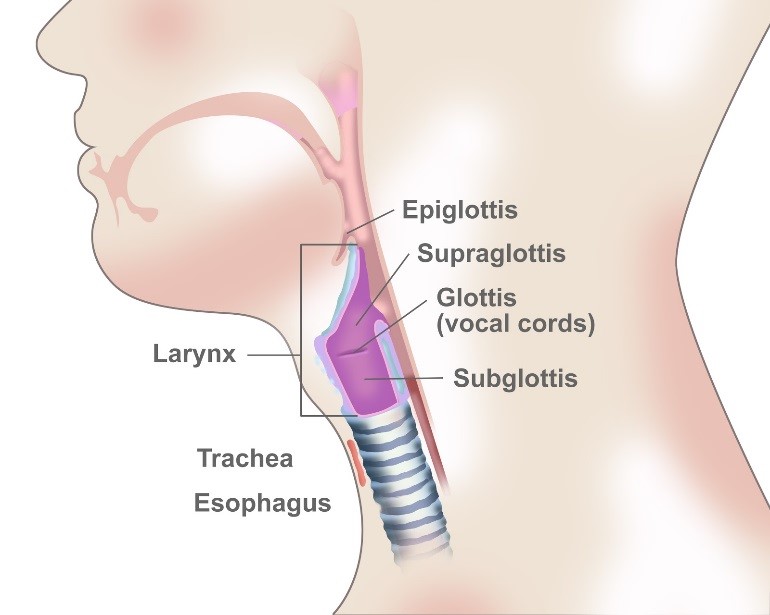
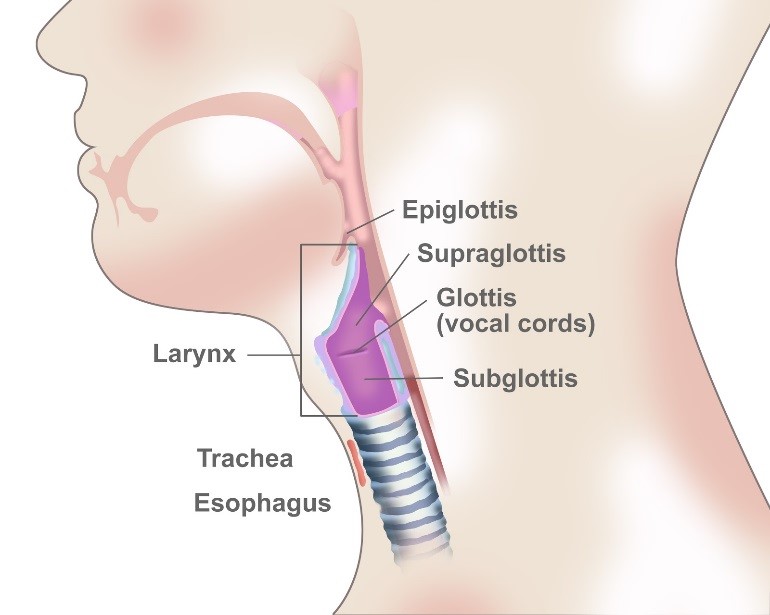
Laryngeal cancer is a disease in which malignant (cancer) cells form in the tissues of the larynx–the part of the throat between the base of the tongue and the trachea. The larynx contains the vocal cords, which vibrate and make sound when air is directed against them. The sound echoes through the pharynx, mouth, and nose to make a person’s voice.
There are three main parts of the larynx, which include:
- Supraglottis – the upper part of the larynx above the vocal cords, including the epiglottis, which is the flap that covers the trachea when swallowing so that food does not enter the lungs.
- Glottis – the middle part of the larynx where the vocal cords are located.
- Subglottis – the lower part of the larynx between the vocal cords and the trachea (windpipe).
Laryngeal cancer is a type of head and neck cancer that forms in squamous cells, which are the thin, flat cells that line the inside of the larynx.
Hypopharyngeal
Hypopharyngeal cancer is a disease in which malignant (cancer) cells form in the tissues of the hypopharynx. It is a type of head and neck cancer.
The hypopharynx is the bottom part of the pharynx (throat). The pharynx is a hollow tube about five inches long that starts behind the nose, goes down the neck, and ends at the top of the trachea (windpipe) and esophagus (the tube that goes from the throat to the stomach ). Air and food pass through the pharynx on the way to the trachea or the esophagus.
Most hypopharyngeal cancers form in squamous cells, the thin, flat cells lining the inside of the hypopharynx. The hypopharynx has three different areas. Cancer may be found in one or more of these areas.